T-Cell Large Granular Leukemia (LGL)
You are here
Definition
T-cell large granular lymphocyte leukemia (T-LGL) exhibits a unexplained, chronic (> 6 months) elevation in large granularlymphocytes (LGLs) in the peripheral blood. It is also known by : Proliferation of large granular lymphocytes (LGLs), LGL leukemia, Tγ-lymphoproliferative disorder, T-cell chronic lymphocytic leukemia.
Sample Cases
Click here for instructions on how to download the free FCS Express Reader to view and manipulate the sample cases.
| Case Name (click on case name to open) |
Comments | Size |
| LGL1 | LGL | 5.44 MB |
| case 29 | variant T LGL This case was kindly provided by the ASCP Press. It is part of Flow Cytometry in Clinical Diagnosis by John Carey, Phil McCoy and David Keren. |
1.37 MB |
| case 17 | LGL This case was kindly provided by the ASCP Press. It is part of Flow Cytometry in Clinical Diagnosis by John Carey, Phil McCoy and David Keren |
1037 kB |
Epidemiology
T-LGL is a rare form of leukemia, which comprises 2-3% of all cases of small lymphocytic leukemias.
Possible causes
Unknown.
Morphology
In periperal blood the neoplastic lymphocytes are large in size with azurophilic granules that contains proteins involved in cell lysis such as perforin and granzyme B. Bone marrow involvement is often present, but to a variable extent. The lymphocytic infiltrate is usually interstitial and/or intrasinusoidal, but a nodular pattern can rarely occur. The leukemic cells of T-LGL can be found in peripheral blood, bone marrow, spleen, and liver. Nodal involvement is rare.
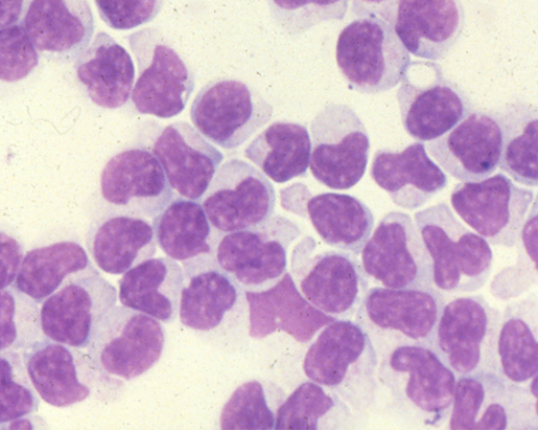 |
| Example morphology of T-LGL lymphocytes from Wright-stained cytospin of ficoled blood lymphs. These cells characteristically have abundant cytoplasm and azurophillic granules. |
Immunophenotyping
T-LGL presents as a predominance of lymphocytes. These cells will display bright CD45 and low SSC and fall into the same region as normal (benign) lymphocytes.
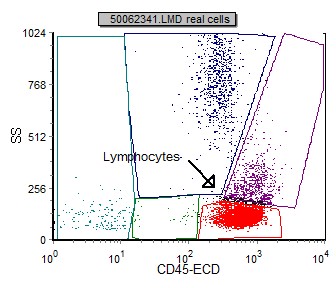 |
| LGL lymphocytes (red) displayed on a CD45 vs SSC gating dot plot. |
In the table below (3) are immunophenotypic markers that are useful in identifying and classifying LGL. The table is stratified into T-LGL and NK-LGL as they display different phenotypes.
| Marker | T-LGL (%) | NK-LGL (%) |
| CD2+ | 100 | 100 |
| CD3+ | 100 | 0 |
| CD5+ | 80 | 0 |
| CD7+ | 83 | 100 |
| All pan T cell Ags + | 63 | 0 |
| CD4+ | 2 | 0 |
| CD8+ | 85 | 21 |
| CD4+/CD8+ | 10 | 0 |
| CD4-/CD8- | 3 | 79 |
| TCR ab+ | 80 | 7 |
| TCR gd+ | 20 | 0 |
| TCR - | 0 | 93 |
| CD11c+ | 44 | 71 |
| CD16+ | 32 | 71 |
| CD56+ | 32 | 71 |
| CD57+ | 95 | 64 |
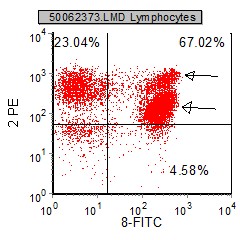
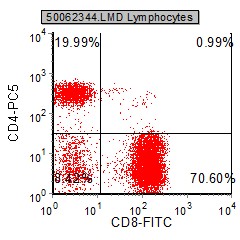
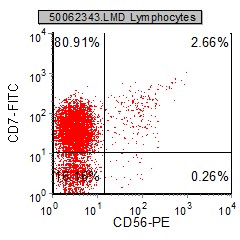
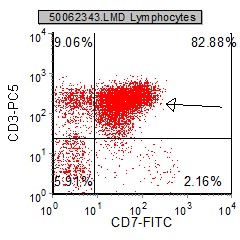
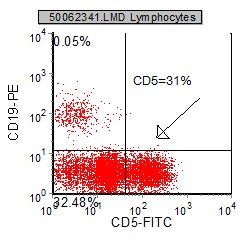
Below are examples of selected dot plots from a case of LGL.
 |
 |
 |
 |
 |
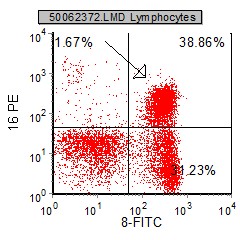 |
| The pan T cell markers CD2, CD7 and CD3 are generally expressed, with a CD8 phenotype. CD4 is usually absent or minimal. | LGL display a predominant CD8 phenotype. The pan T cell markers is usually expressed, but many times one of the T cell markers is aberrantly negative or underexpressed. | CD7 is usually expressed on LGL. The NK markers CD56 and CD16 are usually expressed on about 1/3 of these cases. |
Other relevant tests
Cytochemistry: Immunohistochemistry for perforin, TIA-1, and granzyme B are usually positive.
Genetics: Clonal rearrangements of the T-cell receptor (TCR) genes are a necessary condition for the diagnosis of this disease. The gene for the β chain of the TCR is found to be rearranged more often than the γ chain. of the TCR.
Sub-classification
LGL can be subclassified into T-cell LGL and NK-LGL. The morphology is similar, though the immunophenotype is different.
| Type | Immunophenotype |
|---|---|
| Common type (80% of cases) | CD3+, TCRαβ+, CD4-, CD8+ |
| Rare variants | CD3+, TCRαβ+, CD4+, CD8- |
| CD3+, TCRαβ+, CD4+, CD8+ | |
| CD3+, TCRγδ+, CD4 and CD8 variable |
Flow Diagnosis
The pan T cell markers(CD2, CD3, CD5, CD7) are generally expressed, though frequently one or more are underexpressed or absent. These cells are predominantly CD8 positive, with CD4 negative or minimally expressed. NK markers CD57, CD56 and CD16 are frequently expressed.
References
1. Chan WC, Link S, Mawle A, Check I, Brynes RK, Winton EF. "Heterogeneity of large granular lymphocyte proliferations: delineation of two major subtypes." Blood. 1986 Nov;68(5):1142-53. PMID: 3490288
2. Semenzato G, Zambello R, Starkebaum G, Oshimi K, Loughran TP Jr. "The lymphoproliferative disease of granular lymphocytes: updated criteria for diagnosis." Blood. 1997 Jan 1;89(1):256-60. PMID: 8978299
3. Gorczyca W. Flow Cytometry in Neoplastic Hematology. Informa Healthcare 2007
