Acute Megakaryoblastic Leukemia (AMKL) (M7)
You are here
We are missing a sample case. If you have one, please attach it, or contact us and we will help post it.
Definition
Acute megakaryoblastic leukemia (AMKL) is one form of acute myelogenous leukemia (AML). It is classified as M7 according to the FAB system. AMKL is defined as an AML with >20% blasts, of which 50% or more are of the megakaryocyte lineage.
Sample Cases
Click here for instructions on how to download the free FCS Express Reader to view and manipulate the sample cases.
| Case Name (click on case name to open) |
Comments | Size |
Possible causes
Unknown.
Morphology
Morphologic features include the following:
- Medium- to large-sized megakaryoblasts with round or indented nucleus and one or more nucleoli.
- Agranular, basophilic cytoplasm with pseudopod formation.
- Lymphoblast-like morphology (high nuclear-cytoplasmic ratio) in some cases.
- Circulating micromegakaryocytes, megakaryoblastic fragments, dysplastic large platelets, and hypogranular neutrophils.
- Stromal pattern of marrow infiltration mimicking a metastatic tumor in infants.
- The blast cells vary considerably in size in this aggressive form of leukemia and there is frequent budding of cytoplasmic margins. Auer rod bodies may be found within the neoplastic cells.
M7 blasts are often resemble lymphoblasts, although M7 leukemias may be accompanied by atypical megakaryocytes.
The marrow is often fibrotic.
 |
 |
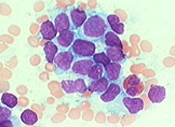 |
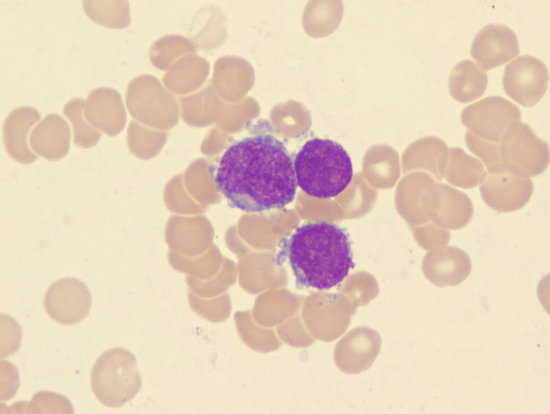
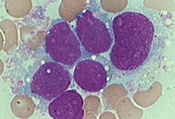
| M7 blasts with pseudopod formation | M7 blasts will shed platelets | M7 blasts clump together |
Immunophenotyping
Immunophenotyping reveals megakaryoblast expression of one or more platelet glycoproteins: CD41 (glycoprotein IIb/IIIa) and/or CD61 (glycoprotein IIIa). Myeloid markers CD13 and CD33 may be positive; CD36 is typically positive. Blasts are negative with the anti-MPO antibody and other markers of myeloid differentiation. In bone marrow biopsies, megakaryocytes and megakaryoblasts may react positively to antibodies for Factor VIII. The differential diagnosis includes minimally differentiated AML, acute panmyelosis with myelofibrosis, ALL, pure erythroid leukemia, and blastic transformation of chronic myeloid leukemia or idiopathic myelofibrosis , and metastatic tumors in the bone marrow (particularly in children).
Other relevant tests
Cytochemistry: Negative stains for SBB and MPO. Blasts reactive with PAS, acid phosphatase, and nonspecific esterase. The blast cells vary considerably in size in this aggressive form of leukemia and there is frequent budding of cytoplasmic margins. Auer rod bodies may be found within the neoplastic cells.
Genetics: No unique chromosomal abnormalities are associated with acute megakaryoblastic leukemia in adults. In children, particularly infants, a distinct clinical presentation may be associated with t(1:22)(p13;q13). The prognosis for this type of acute leukemia is poor.
M7 Variant: Acute myeloid leukemia/transient myeloproliferative disorder in Down syndrome
Individuals with Down syndrome (trisomy 21) have an increased disposition to acute leukemia, primarily the myeloid type. The primary subtype appears to be acute megakaryoblastic leukemia. In cases in which the leukemia remits spontaneously, the process is referred to as transient myeloproliferative disorder or transient leukemia. Clinical features include presentation in the neonatal period (10% of newborn infants with Down syndrome), marked leukocytosis, blast percentage in the blood greater than 30% to 50%, and extramedullary involvement.
Morphologic and cytochemical features include the following:
- Blasts with round to slightly irregular nuclei and a moderate amount of basophilic cytoplasm.
- Coarse azurophilic granules in the cytoplasm that resemble basophil granules.
- Promegakaryocytes and micromegakaryocytes.
- Dyserythropoiesis.
- MPO-negative and SBB-negative blasts.
Immunophenotyping reveals markers that are generally similar to those of other cases of childhood acute megakaryoblastic leukemia.
In addition to trisomy 21, some cases may show other clonal abnormalities, particularly trisomy 8. Spontaneous remission occurs within 1 to 3 months in transient cases. Recurrence followed by a second spontaneous remission or persistent disease may occur. Treatment outcomes for pediatric patients with Down syndrome and persistent disease may be better than those for pediatric patients with acute leukemia in the absence of trisomy 21.
Flow Diagnosis
Flow cytometry characteristically shows moderate CD34, dim CD117, negative to dim HLA Dr, negative CD13, bright CD33and dim CD64, CD41 and CD61. Note of caution when interpreting CD41 and CD61, as they can be expressed with platelet absorption on other cells.
Note: CD42b is strongly expressed on platelets, but not expressed on megakaryoblasts.
