Acute Promyelocytic Leukemia - AML with t(15;17)(q22;q12)
You are here
Definition
Acute promyelocytic leukemia is a subtype of acute myelogenous leukemia (AML), a cancer of the blood and bone marrow. It is also known as acute progranulocytic leukemia; APL; AML with t(15;17)(q22;q12), PML-RARA and variants; FAB subtype M3 and M3 variant. In APL, there is an abnormal accumulation of immature granulocytes called promyelocytes. The disease is characterized by a chromosomal translocation involving the retinoic acid receptor alpha (RARα or RARA) gene and is unique from other forms of AML in its responsiveness to all trans retinoic acid (ATRA) therapy.
Sample Cases
Click here for instructions on how to download the free FCS Express Reader to view and manipulate the sample cases.
| Case Name (click on case name to open) |
Comments | Size |
| M3_1 | APL | 2.97 MB |
| M3_2 | APL (hypogranular) | 9.34 MB |
| M3_3 | APL (hypergranular) | 6.82 MB |
| case 19 | M3v with t(15;17) This case was kindly provided by the ASCP Press. It is part of Flow Cytometry in Clinical Diagnosis by John Carey, Phil McCoy and David Keren. |
1569 kB |
Epidemiology
Acute promyelocytic leukemia (APL) represents 5-8% of AML in adults. The median age is approximately 40 years, which is considerably younger than the other subtypes of AML (70 years). The incidence is increased in patients originated in Latin American countries
Possible causes
Similar to ALL, possible factors that have been associated with AML (and MDS) are viruses, radiation, cytotoxic chemotherapy and benzene exposure. Exposure to the atomic bomb of WWII increased the incidence of all leukemias including AML. In addition, smoking is attributed to an increased risk.
Morphology
There are two subtypes of APL based on morphologic features; hypergranular and microgranular (hypogranular).
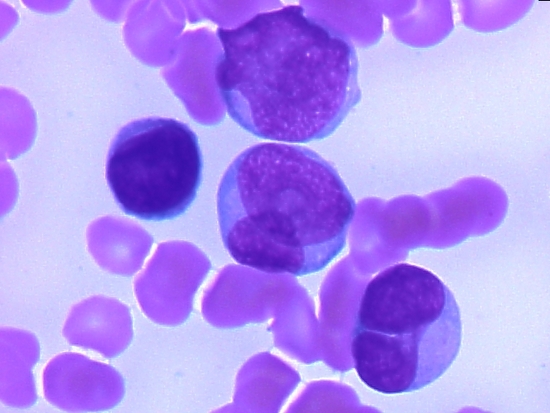
- Hypergranular APL blasts vary greatly in size. The cytoplasm is densely packed with large granuoles occassionally obscurring the nucleus. Characteristic Auer rods or bundles of Auer rods are frequently present. (left image)
- Microgranular/Hypogranular APL blasts have distinct morphologic features such as bilobed nucleus and paucity or absence of granules. many times these cells are confused with monoblasts. (right image)
 |
|
| Morphological example of a hypergranular myeloblast in APL. Note the azurophillic granuoles and Ayer rods. | Morphologic example of a hypogranular myeloblast in APL. Note the lack of granuoles and bilobed nucleus. |
Immunophenotyping
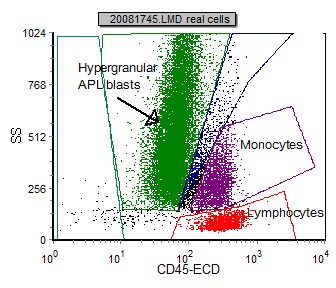
Blasts in APL can be initially identified using a SSC vs CD45 plot. As noted by the differences in morphology, different subtypes of APL exhibit different CD45 vs SSC plots. Correlation to morphology is important as hyperganular APL blasts generally fall in the same region as normal granulocytes. Hypogranular APL blasts have a lower SSC. Note the correlation with morphology.
 |
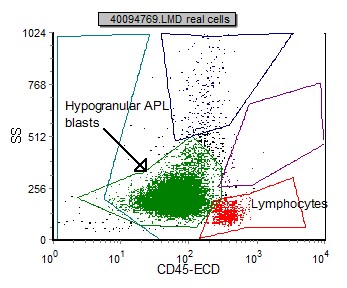 |
| Ths CD45 vs SSC dot plot corresponds to the above hypergranular APL blast. Note the location of the green population. | Ths CD45 vs SSC dot plot corresponds to the above hypogranular APL blast. Note the location of the green population. |
Once the blasts are identified and gated, the following markers are useful in classification of APL. Please note flow cytometry is not diagnostic for APL, and must be confirmed with retinoic acid receptor-alpha (RARα) :
| Marker or parameter | APL hypergranular | APL hypogranular |
| SSC | markedly increased | decreased (blast region) |
| CD2 | 23% (dim) | 90% (dim to mod) |
| CD4 | 27% (dim) | 50% (dim) |
| CD11b | 0% (occassional subset) | 0% |
| CD11c | 6% (dim) | 0% |
| CD13 | 0% | 100% (dim to mod) |
| CD14 | 0% | 0% |
| CD16 | 0% | 0% |
| CD19 | 0% | 0% |
| CD33 | 100% (mod to bright) | 100% (bright) |
| CD34 | 2% (occassional subset) | 75% |
| CD45 | 100% (moderate) | 100% (moderate) |
| CD56 | 15% | 20% |
| CD64 | 70% (dim) | 90% (dim) |
| CD117 | 100% (moderate) | 100% (moderate) |
| HLA Dr | 0% | 0% |
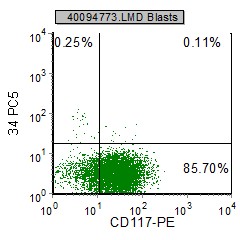
Example APL histograms:
 |
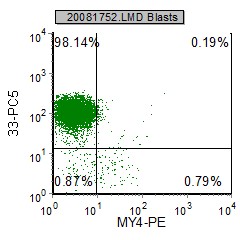 |
 |
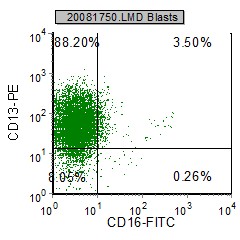 |
| CD34 and HLA Dr are characteristically negative in APL. CD13 and CD117 are usually positive. | CD33 and CD13 are expressed in APL. CD16 and My4 are not. |
Other relevant tests
Genetics: Acute promyelocytic leukemia is characterized by chromosomal translocation involving the retinoic acid receptor-alpha gene on chromosome 17 (RARα). In 95% of cases of APL, retinoic acid receptor-alpha (RARα) gene on chromosome 17 is involved in a reciprocal translocation with the promyelocytic leukemia gene (PML) on chromosome 15, a translocation denoted as t(15;17)(q22;q12). Four other gene rearrangements have been described in APL fusing RARα to promyelocytic leukemia zinc finger (PLZF), nucleophosmin (NPM), nuclear matrix associated (NUMA), or signal transducer and activator of transcription 5b (STAT5B) genes.
Sub-classification
APL exists as two types, hypergranular or typical APL and microgranular (hypogranular) APL. APL comprises 5% to 8% of cases of AML and occurs predominately in adults in midlife. Both typical and microgranular APL are commonly associated with disseminated intravascular coagulation (DIC). In microgranular APL, unlike typical APL, the leukocyte count is very high with a rapid doubling time.
Flow Diagnosis
The myeloid markers CD33 and CD117 are positive. CD13 and CD34 are generally positive in the hypogranular variant. HLA Dr is characteristically negative (unlike other AMLS)
